In today’s world of selfies, filters, and constant exposure to beauty ideals, many people feel pressure to look their best. Non-surgical cosmetic procedures such as Botox, dermal fillers, and skin treatments are now widely accessible, offering quick results with little downtime. For many, these treatments boost confidence and provide a welcome refresh.
But for some individuals, concerns about their appearance go much deeper than a few wrinkles or fine lines. When worries about perceived flaws become overwhelming, persistent, and life-disrupting, the issue may not be cosmetic at all — it may be Body Dysmorphic Disorder (BDD).
Understanding BDD is essential for both patients and practitioners in aesthetics. Let’s explore what it is, how it affects decision-making around treatments, and why recognising it matters so much.
What Is Body Dysmorphic Disorder?
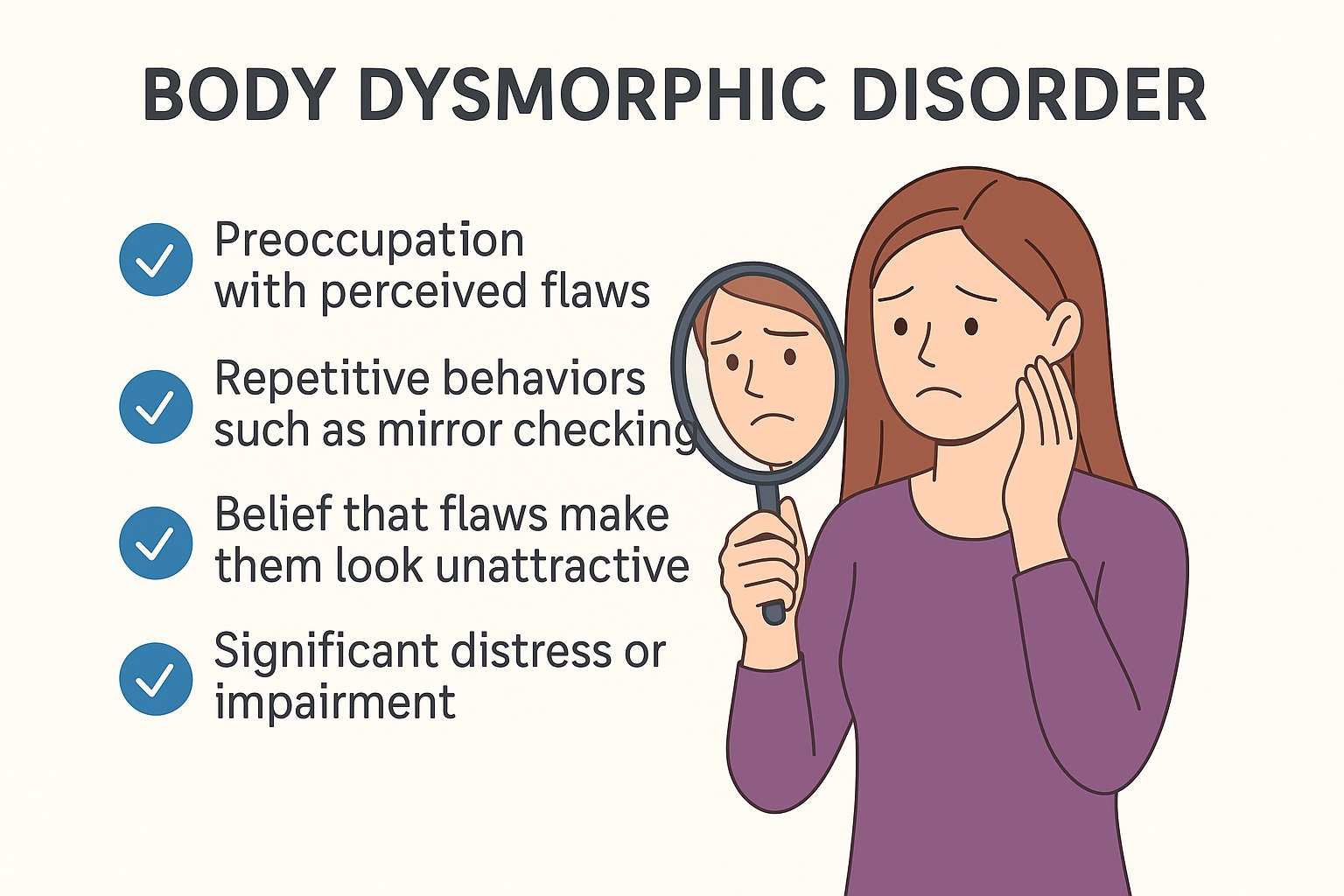
Body Dysmorphic Disorder is a recognised mental health condition where a person becomes excessively preoccupied with one or more perceived flaws in their appearance. These flaws are often minor or even invisible to others, but to the person affected, they feel significant and distressing.
BDD is classified under obsessive–compulsive and related disorders in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders). It is not a matter of vanity. Rather, it is a serious psychological condition that can impact every aspect of life, from relationships and socialising to work and self-esteem.
Signs and Symptoms
BDD can look different from person to person, but common features include:
- Persistent preoccupation with perceived defects in appearance (e.g., skin, nose, lips, body shape).
- Repetitive behaviours such as mirror checking, excessive grooming, seeking reassurance, or comparing oneself to others.
- Avoidance behaviours such as avoiding mirrors, cameras, social situations, or bright lights.
- Emotional distress including anxiety, shame, or depression linked to body image.
- Functional impairment — daily life, relationships, or work may suffer.
Importantly, many individuals with BDD believe that cosmetic treatments will “fix” the problem. However, the distress comes from their perception rather than the actual appearance, meaning that procedures rarely provide lasting relief.
BDD and the Aesthetics Industry
The aesthetics industry is built on improving appearance. For someone with BDD, this can seem like the perfect solution. They may repeatedly seek Botox, fillers, or surgery in the hope that changing a specific feature will resolve their distress.
But here’s the key issue:
- Cosmetic treatments cannot cure BDD.
- In fact, they can sometimes make things worse. If the underlying perception is distorted, even the best results may leave the patient dissatisfied.
- Some individuals may hop from clinic to clinic, chasing procedures that never deliver the emotional relief they seek.
This creates a challenge for practitioners: knowing when a patient’s concerns are genuine and reasonable, and when they may be symptomatic of BDD.
Why Recognition Matters
For practitioners, recognising potential BDD is not just about ethics — it is about patient safety. Treating someone with BDD can lead to:
- Dissatisfaction and complaints: Even good results may be viewed negatively by the patient.
- Psychological harm: Procedures can reinforce the cycle of obsession and distress.
- Reputational risk: An unhappy patient may blame the clinic for not meeting unrealistic expectations.
From the patient’s perspective, undergoing unnecessary or repeated treatments can:
- Drain financial resources.
- Cause physical risks such as scarring, asymmetry, or complications.
- Delay access to the real help they need — mental health support.
Assessing Patients in Aesthetics
Responsible practitioners don’t simply provide treatments on demand. A proper consultation should always include a discussion of motivations, expectations, and mental health.
Screening for BDD may include questions such as:
- How long have you been concerned about this feature?
- How much time each day do you spend thinking about it?
- How does it affect your daily life?
- Have you sought multiple opinions or treatments for the same concern?
- What result are you expecting from treatment?
Red flags may include:
- Disproportionate distress about a minor flaw.
- A history of repeated procedures with ongoing dissatisfaction.
- Unrealistic expectations (“I want to look perfect” / “This will change my life completely”).
- Strong emotional reactions during consultation.
If BDD is suspected, the ethical approach is to decline treatment and gently guide the patient towards professional psychological support.
Treatment for BDD
While aesthetic treatments are not effective, there are evidence-based therapies that can help:
- Cognitive Behavioural Therapy (CBT): Specially adapted CBT for BDD helps patients challenge distorted thoughts and reduce compulsive behaviours.
- Medication: Selective serotonin reuptake inhibitors (SSRIs) are often prescribed to manage symptoms.
- Support networks: Encouragement from family, friends, and support groups can play an important role in recovery.
Raising awareness within the aesthetics community ensures that patients with BDD are identified and directed towards these more appropriate treatments.
The Practitioner’s Responsibility
The General Medical Council (GMC) and other professional bodies in the UK emphasise that practitioners must:
- Ensure patients are making informed, autonomous decisions.
- Refuse treatment if it is not in the patient’s best interest.
- Prioritise patient wellbeing over financial incentives.
This aligns with a broader shift in aesthetics: from a purely cosmetic service to a healthcare-based practice that considers both physical and psychological wellbeing.
Advice for Patients
If you are considering aesthetic treatments, ask yourself:
- Am I bothered by a feature that others barely notice?
- Do I spend hours thinking about it or checking mirrors?
- Do I believe a procedure will solve deeper issues in my life?
- Have I already had treatments and still feel unhappy?
If you answered yes to several of these, it may be worth speaking to a GP or mental health professional before seeking further aesthetic treatments. Addressing underlying concerns can lead to more lasting confidence than any injection or surgery.
Conclusion
Body Dysmorphic Disorder is more common than many realise and can have a significant impact on the aesthetics industry. While Botox and fillers can provide excellent results for suitable patients, they cannot resolve the distorted self-image at the heart of BDD.
For practitioners, recognising and managing BDD ethically protects both patients and the profession. For patients, understanding the difference between normal aesthetic concerns and BDD can prevent disappointment and encourage the right type of support.
Aesthetics should always enhance confidence — but true confidence starts with mental wellbeing.