Introduction
In recent years, non-surgical rhinoplasty — often marketed as the “liquid nose job” — has gained immense popularity. The promise is tempting: a quick, minimally invasive procedure that can subtly reshape the nose using injectable fillers, all without the risks or downtime of surgery. Social media has amplified this trend, showcasing dramatic before-and-after photos that make the procedure look safe, simple, and accessible.
However, beneath the surface lies a harsh reality that is rarely discussed outside of medical circles. Despite being formally trained and qualified in this procedure, I have made a deliberate decision not to perform non-surgical rhinoplasty in my practice. The risks, in my view, outweigh the benefits, and I believe it is my ethical responsibility to protect patients from harm, even when it means saying no.
Understanding Non-Surgical Rhinoplasty
Non-surgical rhinoplasty involves injecting dermal fillers (commonly hyaluronic acid-based products) into precise areas of the nose to improve its shape. The procedure can:
- Camouflage bumps or asymmetries.
- Create the illusion of a straighter nose.
- Lift or define the nasal tip.
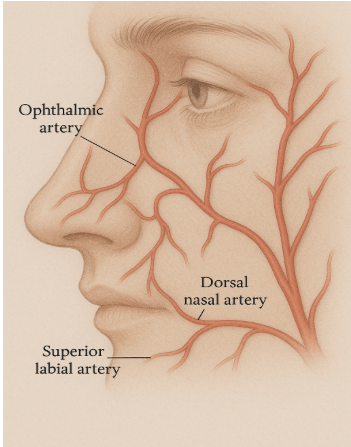
While marketed as “non-invasive,” the reality is that it involves injecting into a region of the face with extremely complex and delicate vascular anatomy. The nose is not only cosmetically important but also medically high-risk due to its blood supply and proximity to critical structures like the eyes and brain.
The Real Risks of Non-Surgical Rhinoplasty
1. Blindness
The most devastating complication is sudden, irreversible blindness. If filler accidentally enters a blood vessel, it can travel retrograde into the ophthalmic artery, cutting off blood supply to the retina. Within minutes, the damage is permanent.
- Blindness from filler injection is not just theoretical — hundreds of documented cases exist worldwide.
- No doctor, no matter how skilled, can guarantee zero risk.
2. Skin Necrosis
Another serious complication is skin necrosis, where injected filler blocks blood flow, leading to tissue death. This can result in painful ulceration, permanent scarring, and even disfigurement of the nose. What begins as a “quick fix” can end with devastating cosmetic and psychological consequences.
3. Vascular Complications Beyond the Nose
Because the nasal blood vessels communicate with the brain, filler embolism can theoretically lead to stroke. Though rare, this possibility underscores how high-stakes the procedure really is.
4. False Sense of Safety
Many patients mistakenly believe non-surgical rhinoplasty is “risk-free” because it doesn’t involve scalpels, anesthesia, or downtime. This misconception is often reinforced by social media influencers who showcase only the highlights, while the serious complications remain hidden.
Despite my training and competency in performing non-surgical rhinoplasty, I have chosen to exclude it from my practice. Here’s why:
1. The Stakes Are Too High
In aesthetic medicine, every procedure carries some degree of risk. But the risk-benefit ratio matters. When a treatment has the potential to cause irreversible blindness for a primarily cosmetic gain, I cannot ethically justify offering it.
2. Ethical Responsibility to Patients
As physicians, we must prioritize patient safety above all else. While patients may request this procedure, it is my duty to guide them toward safe, evidence-based choices. I would rather say “no” than risk harming someone under my care.
3. Safer Alternatives Exist
For patients seeking nasal refinement, traditional surgical rhinoplasty — while more invasive — allows for controlled, permanent results without the same vascular risks. Alternatively, makeup techniques or even minor surgical adjustments can achieve improvements without exposing patients to the unique dangers of fillers in the nose.
- Avoiding False Reassurance
Performing this procedure would, by default, lend credibility to the notion that it is safe. By refusing to perform it, I hope to send a clear message: popularity does not equal safety.
The Allure vs. The Reality
The rise of non-surgical rhinoplasty reflects broader cultural trends: the demand for quick fixes, the influence of Instagram aesthetics, and the normalization of cosmetic procedures among younger generations. Unfortunately, what’s lost in the conversation is the true medical reality.
- Social media shows flawless results in 15-second clips.
- Rarely do we see the complications: the patient who lost vision, the one left with scarring, or the one who suffered months of reconstructive treatments after a “simple” filler injection.
As a physician, I have seen the darker side of aesthetics — the outcomes that don’t make it to social media. And that knowledge shapes how I practice medicine.
What Patients Should Know
If you are considering non-surgical rhinoplasty, please keep the following in mind:
- Ask about risks honestly. If your provider glosses over blindness or necrosis, that’s a red flag.
- Choose qualified providers. At minimum, ensure your injector is a licensed medical professional with advanced training in facial anatomy. If the worst happens, your practitioner will need to act FAST. Non medics will not have access to the required emergency drugs.
- Have realistic expectations. Non-surgical rhinoplasty cannot make your nose smaller; it can only camouflage irregularities by adding volume.
- Consider long-term outcomes. Fillers may migrate, distort the shape of your nose over time, or require repeated treatments.
Conclusion
Non-surgical rhinoplasty is often marketed as a simple, lunchtime procedure with instant results. But beneath the glossy advertising lies a stark reality: this is a high-risk procedure with life-changing potential complications.
As a physician, I believe my first responsibility is to protect patients from harm. That is why, despite being trained in this technique, I have chosen not to perform it. For me, no cosmetic improvement can ever justify the possibility of causing blindness, necrosis, or worse.
By speaking out, I hope to raise awareness and empower patients to make informed, safe choices when it comes to their health and appearance.
Sometimes, the safest choice is not to perform the procedure at all.